Revenue Cycle Management (RCM) — Biller Dashboard & Billing Settings
My Role
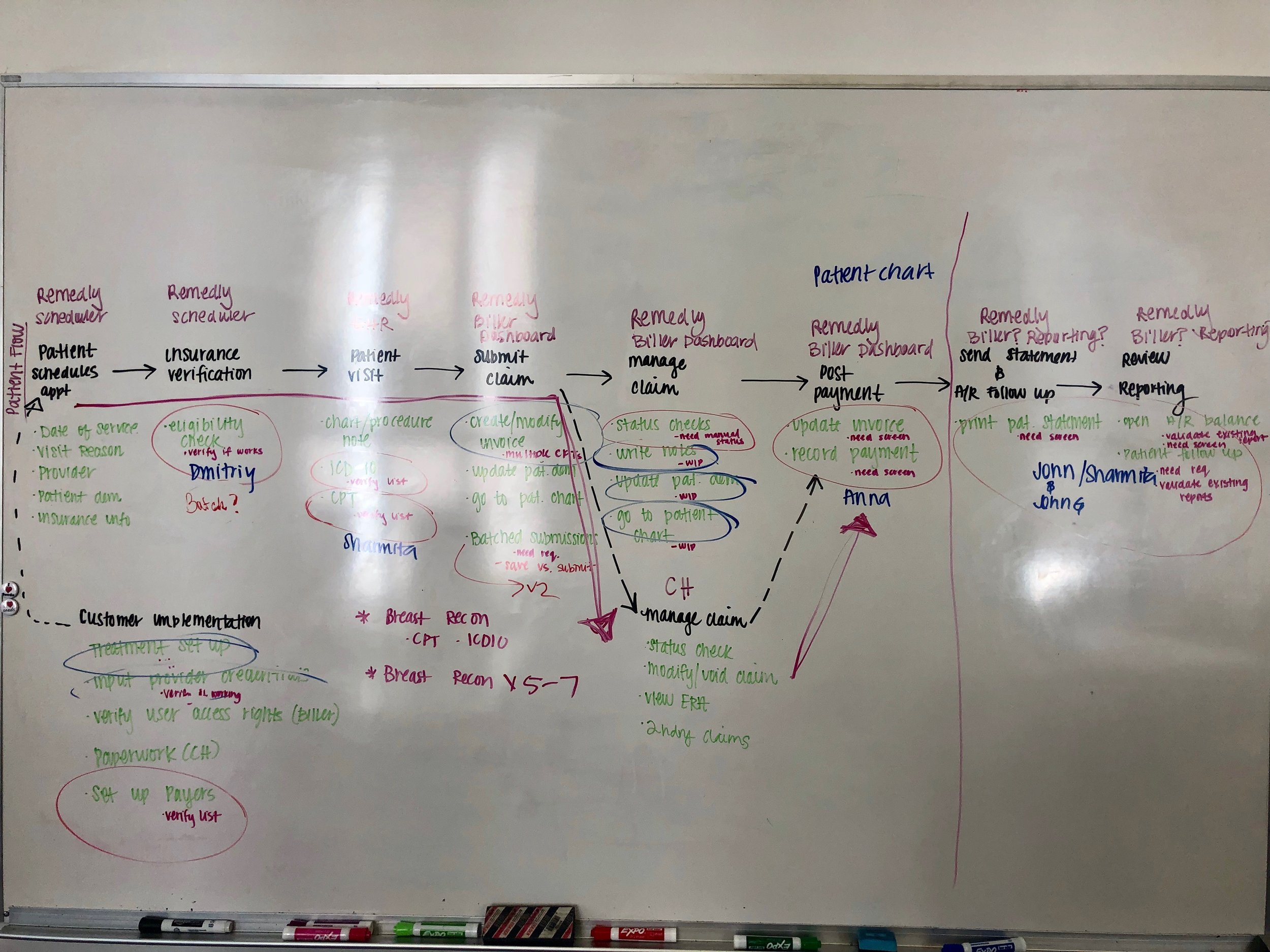
UX research & domain discovery
Stakeholder and biller interviews
Workflow modeling & information architecture
Wireframing and high-fidelity prototyping
Cross-functional collaboration
EXISTING DESIGN
FINAL DESIGN


PROBLEM STATEMENT
Revenue Cycle Management (RCM) is the financial backbone of medical practices—tracking patient care from registration and scheduling through claim submission and final payment.
However, the existing RCM experience failed to support the full billing lifecycle required by modern medical practices. Core workflows were fragmented, difficult to manage at scale, and misaligned with how billers actually work—leading to inefficiencies, errors, and delayed revenue.
PROJECT GOAL
Design a new Biller Dashboard and Billing Settings experience that:
Supports end-to-end billing workflows
Introduces new, high-impact billing features
Improves visibility, control, and efficiency for billers
Reduces manual work and cognitive load
Stage 1 | Research
Given my limited initial exposure to Revenue Cycle Management, I started by building a research foundation to deeply understand the domain before designing solutions.
Research Objectives
Understand what RCM is and how billers use it day to day
Identify billers’ needs, pain points, and mental models
Analyze how existing medical software supports billing workflows
Methods
Conducted interviews with internal and external billing teams
Walked through the entire billing lifecycle, from intake to claim resolution
Documented real workflows, edge cases, and failure points
Key Insight
Billing is not a linear process—it is iterative, exception-driven, and time-sensitive, requiring dashboards that surface priorities, not just data.
KEY FINDINGS

COMPETITOR ANALYSIS
I evaluated billing solutions from leading medical software platforms, focusing on:
Claim management workflows
Feature depth and customization
Information hierarchy and UI clarity
Error prevention and recovery patterns
This analysis helped identify:
Industry best practices worth adopting
Gaps where competitors overcomplicated workflows
Opportunities to differentiate through usability and clarity

Stage 2 | Ideation
To fully understand Remedy’s billing ecosystem, I created a detailed sitemap and process flows covering the entire billing cycle.
Outcomes
Visualized how billing tasks interconnected across the system
Identified redundant steps and manual workarounds
Surfaced critical pain points and opportunities for automation
This step was instrumental in shifting the design from feature-based to workflow-driven.


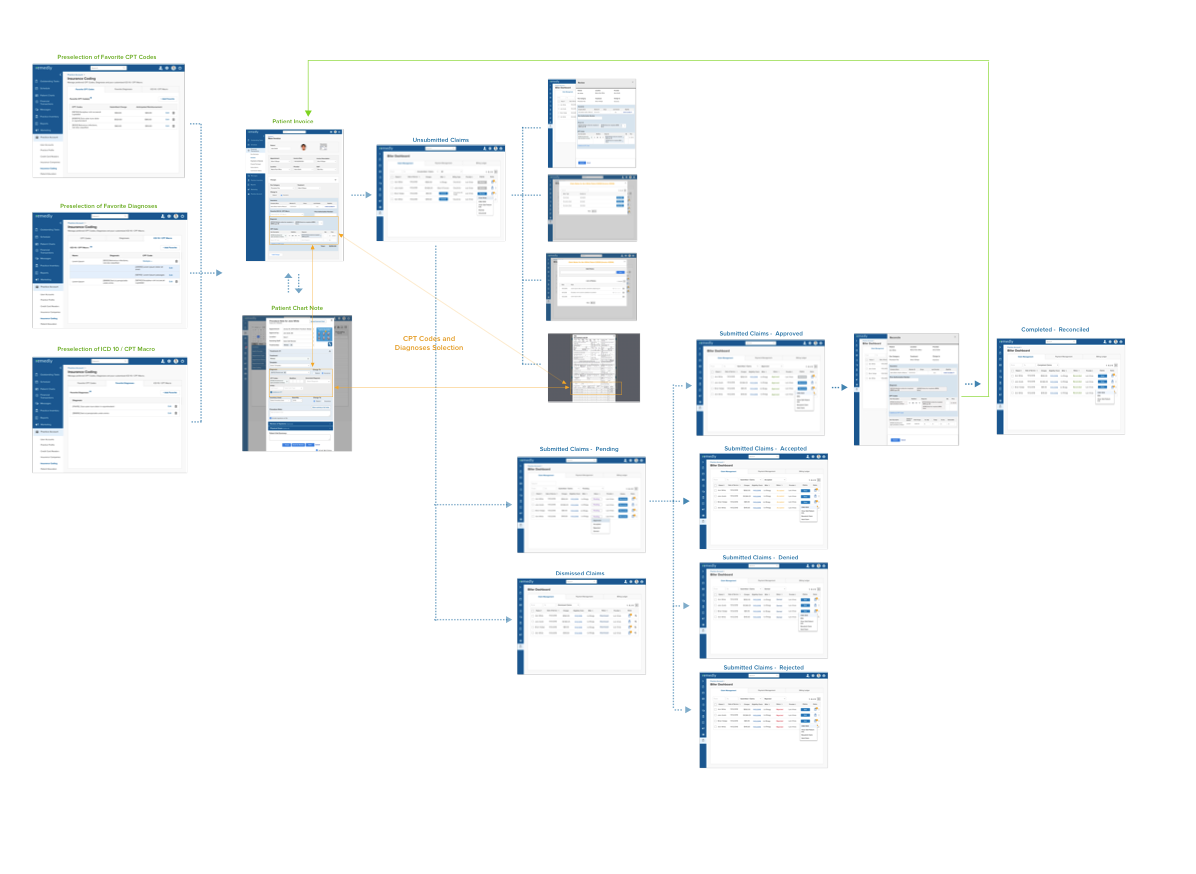
Stage 3 | Design
Using insights from research and flows, I designed task-focused wireframes for key billing scenarios.
Design Principles
Reduce cognitive load for high-frequency tasks
Prioritize clarity and speed over density
Make system status and next actions immediately visible
Support both novice and expert billers
Each iteration was validated against real billing workflows to ensure accuracy and compliance.
Stage 4 | Prototype
I created a high-fidelity interactive prototype in InVision to validate end-to-end workflows.
Key Flows Included
Creating and managing favorite CPT, ICD-10, and diagnosis codes
Building reusable CPT / ICD macros
Managing claims through the Biller Dashboard
Reviewing claim status, errors, and next actions
The prototype allowed stakeholders and billers to experience the redesigned workflows before development.
OUTCOME
Delivered a redesigned RCM experience aligned with real-world billing practices
Improved efficiency and clarity for billers managing complex claim workflows
Established a scalable foundation for future billing enhancements
Reduced reliance on manual processes and institutional knowledge
(Translation: fewer billing errors, faster claims, happier billers.)